With its microscopic size and lethal strength, fentanyl has emerged as a formidable force in the landscape of drug misuse. It was invented in 1959 by Paul Yonson as the “perfect hospital drug.” The effects of fentanyl don’t last as long, allowing patients to get in and out of hospitals. Less than ten years ago, the Drug Enforcement Administration (DEA) reported that no drug users wanted fentanyl. It was too potent and the death rate was too high. However, only one year after this report, fentanyl was killing more people than any other drug in the United States, totaling almost 20,000 victims in just 2016. The current severity of the fentanyl epidemic was entirely unanticipated.
In the 1990’s oxycontin was being prescribed at an alarming rate due to it being advertised as less addictive than other opioids. However, many people began abusing the medication by crushing the pills to make them more potent. In 2010, the producer of oxycontin, Purdue Pharma, stopped making the opioid. With this banning of oxycontin, many addicted people turned to heroin. However, there wasn’t a big enough supply of heroin to meet the demand, forcing people to seek out drugs that had a similar effect, like fentanyl.
Even though fentanyl isn’t appealing to users, it’s incredibly attractive to drug dealers. Fentanyl is synthetic and made in labs, making it an opioid. Opioids are much cheaper and easier to manufacture compared to opiates, which are natural and mainly derived from the opium poppy plant. Examples of opiates include oxycontin, heroine, and morphine. Opioid, sometimes considered an umbrella term for both opioids and opiates, work by latching onto the Mu receptor. This linkage makes us feel the same pleasure we do when completing basic life functions, like eating. However, this pleasure in the absence of severe pain motivates us to take opioids again, causing addiction. Opioids stop the electrical pain signals, which is why fentanyl is typically prescribed after major surgeries and as a treatment for severe pain. When opioids enter the midbrain, which is the reward section of the brain, they generate a signal that releases dopamine. This causes our brain to associate these happy feelings with the circumstances they happened in, leading to addiction. You eventually form a tolerance and become dependent on opioids, causing your performance to drop without drugs present. Psychology Teacher Mr. Mellon explained tolerance by saying, “After prolonged drug use the brain becomes less sensitive to natural ways of releasing dopamine and relies even more on the drug to get that reward.”

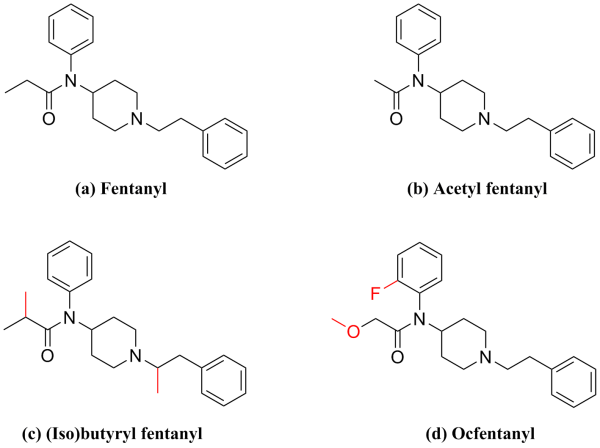
Fentanyl is a white powder and is hard to discern from heroin and cocaine, which is why they are drugs fentanyl is commonly mixed with. It’s much cheaper for dealers and more addictive, so they get more consistent buyers. Most users don’t even realize they’re taking fentanyl. Some of their clients might die, but it’s more lucrative for drug dealers in the long run to lace other drugs with fentanyl. The majority of fentanyl is sourced from China, where it was quasi-legal up until five years ago. On May 1, 2019, China officially banned all forms of fentanyl. Previous to this announcement, fentanyl analogs were extremely common. These are slightly altered forms of fentanyl, which were technically legal. One of our chemistry teachers, Mr. Jadonath, described fentanyl analogs as “illicit and often deadly-alterations of the medically prescribed drug fentanyl. The analogs have similar, but not the same chemical structure, and they mimic the pharmacological effects of the original drug.” Even considering this ban, most of the United States’ illicit supply of fentanyl still originates in China, where it’s then smuggled into the US through Mexico.
Portals)
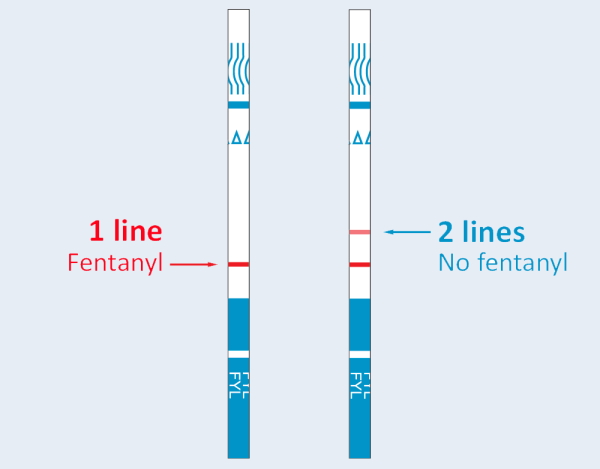
The European Union estimates that the amount of fentanyl required to overdose is 2 milligrams. One way to prevent a fentanyl overdose is a fentanyl test strip (FTS). FTS are small, clear pieces of paper that can detect the presence of fentanyl in drugs. However, Naloxone has saved countless lives after an overdose has occurred. Naloxone is a drug that reverses the effects of an opioid overdose, and has no effect on someone without opioids in their system. It was recently approved for over-the-counter sale. It currently comes in two forms, a nasal spray (under the brand name of Narcan) and injections, which are inserted under the skin, into the muscle, or into the veins. Signs of an overdose include vomiting, unconsciousness, small pupils, as well as purple lips and fingernails.

In Miami-Dade county, students are beginning to be taught the signs of overdose and how to administer Narcan. The FDA reported that fentanyl overdoses among teens aged 14-18 increased by 94% from 2019 to 2023 and that Florida was ranked second in the nation for fentanyl-related deaths this year. Fortunately, our school nurse, Nurse Anthony, reported that APK does not have a fentanyl problem. We do however, as I’m sure most students know, “have an ongoing battle with marijuana use.” One of our student interviewees explained that they’re unsure if fentanyl awareness should be taught at school: “It’s highly dangerous and kills a lot of teens who don’t even know they’re using fentanyl because it gets mixed in with what they consider ‘harmless’. However, if kids were educated about this more, it means they’re getting exposed to it.” Although some of our interviewees had different opinions, one thing they all agreed on was that APK is not doing enough to combat drug use in our school. Mr. Talbert, another chemistry teacher, explained, “I think drug usage is a big issue that we have, and the problem that we have is that we lack proper disciplinary reactions to things.” For many students, the reward granted by the drug-induced high is greater than the risk of discipline. Mr. Jadonath suggested “providing students with support and programs to help them.”
The symptoms of an Opioid Use Disorder (OUD) may include a strong craving for opioids, continuing to use opioids in dangerous situations, and an opioid tolerance. If you or someone you know is struggling with a drug problem, contact the SAMHSA National Helpline at 1-800-662-4357.